“A lack of MSK leadership” Go on, explain yourself.
After JC started the discussion on MSK reasoning, responsibility and reform with #TheBigRs I wrote my feedback in blog form. The main thrust of this (if I can say thrust without everyone laughing) was to articulate the overall feeling that I have had for a while that our profession doesn’t always appear fit for the purposes that it is being used for. If anything I left #TheBigRs with this enhanced and emboldened as I felt that this was a more broadly held belief than by just grumpy old me.
I finished the blog with some questions about how, as a profession, we should move forward, suggesting that I couldn’t see where this leadership would come from. Individual service providers aside.
This blog was greeted with lots of Twitter activity, which frankly made me nervous and annoyed my better half, as my phone didn’t let up. It also posed some really interesting questions. In this time of RESPONSIBILITY about REFORM I thought I couldn’t really leave my opinions hanging and will take this opportunity to clarify.
There was a lot of interest in my lack of confidence in the CSP. Some of this is born out of the fact that through Frontline the CSP have been slowly torturing me with mundanities for the last 22 years. When I have needed them for professional support as a union they have been found lacking (e.g. their agreement to the policy of increment freezing). But mainly as I couldn’t see that what needs to be done was being actioned. This might be because I only take the wrapping off Frontline as I am a diligent recycler. If however through this blogging I am proven wrong, that we can say that our future is in strong hands then I will be more than happy.
I do give my opinion in a kind of “who the hell am I and who listens to me anyway” kind of way. But I am keen to show responsibility for my profession. So here it is.
In a very broad brushed sense in my last blog I outlined what I felt good MSK practice looks like. You will notice that I haven’t included anything in the way of technical skills, by which I mean the ability to perform a certain clinical test or rehab program. Not because I do not think they are important, but because they are technical skills and can be reproduced easily. They are however easy to demonstrate, critically appraise and develop and are therefore too often the mainstay of many competency documents.
"When I undertake second opinions in my clinical practice, I would be very worried if the only thing I could add to the picture was an awesome McMurrey’s."
As a profession we happily outsource a lot of our learning and development to University’s. Since my BSc in Bradford I have done an MSc at Manchester Met, Injection Therapy at University of Keele and laterally Independent Prescribing at University of York. I’ve written reflective portfolios, essays, sat exams and done OSCEs all of which have made me read and have added something. However if I think about the times I have really progressed in my career it is when I have been subjected to patients and had my practice scrutinised. MACP placements, taking patients to be reviewed by an MSK physician, working in orthopaedic clinics, peer review. These experiences have occurred throughout my career at different times when I have been able to take different aspects from them based upon where I was at the time in my clinical journey.
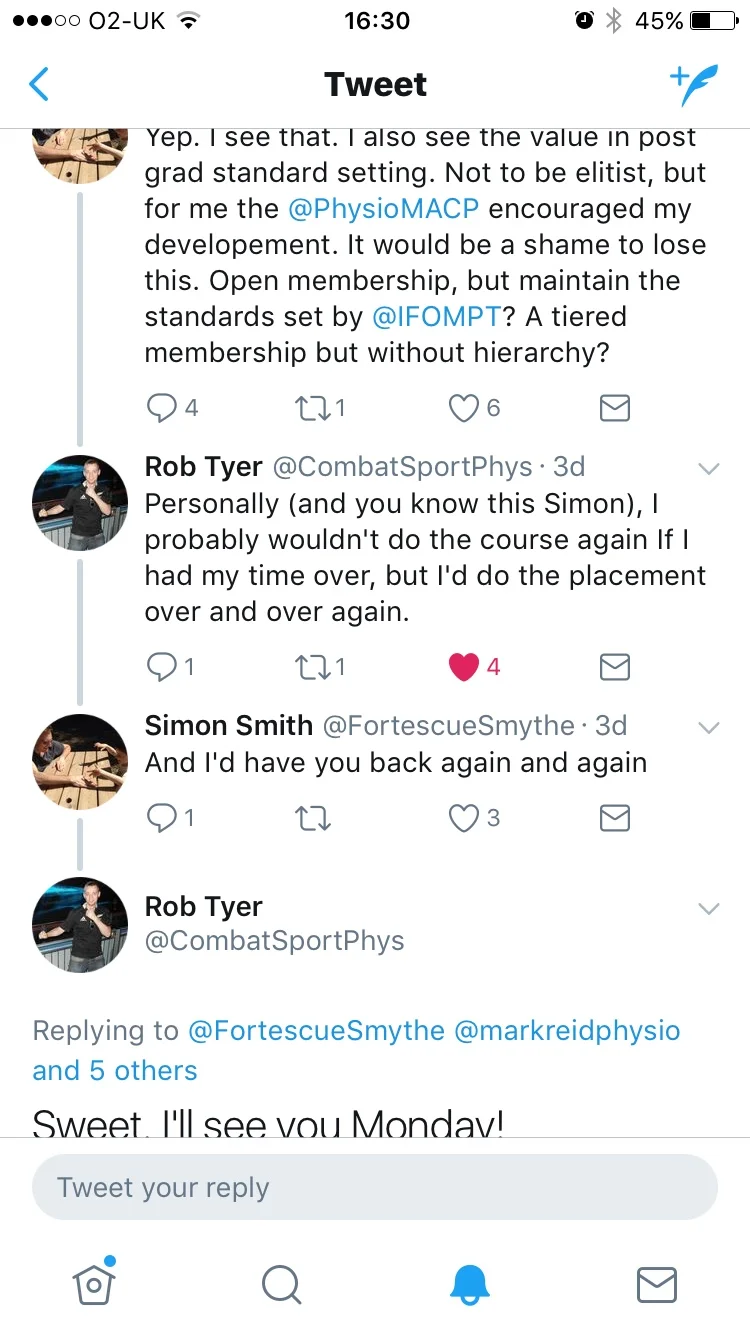
The Physio Matters very own Rob Tyer expressed this in Tweet form very well. Throughout all of his MACP/MSc process it was the clinical placements that he gained the most from. I’d definitely have him back, but I might get a gagging order in place first!
To take this back to the question at hand, we then have to look at the breadth of experience needed to develop Neil 2.0, or indeed any proficient MSK practitioner.
In a first contact practitioner role we will come across tendinopathy, arthropathy, acute and chronic soft tissue stuff; your basic MSK issues. We’re good at them us physios.
However we will also come into contact with undiagnosed rheumatology cases, missed trauma needing orthopaedic intervention, neuropathy and god forbid those pesky masqueraders; serious pathology pretending to be a nice simple MSK presentations.
If our ability to recognise these cases is an important part of the triage process a first contact practitioner is required to do, should exposure to this in anything other than an academic sense be left up to chance?
Once you’ve seen one septic arthritis, you’ll know another when you see it. When you see a spinal fracture that’s been missed in A&E due to a lack of bony tenderness, you’ll know the importance of developing a narrative relating to onset. How significant force is reported by a patient after the fact is a useful lesson.
My point being that for years medics have been developing their clinical skills through a well defined process. They specialise after a good generalist grounding, and then enter a process of on the job training that has an expectation of development until they reach a point when an external body decides their clinical practice is at a level that they can be deemed as a consultant. They then continue to learn and to disseminate their knowledge.
Lets look at our career gateways:
State registration (MCSP) - This is the start of our journey, we get this at the beginning of our careers. Realistically it sets us apart from other non-qualified ‘therapists.’ It says nothing about our speciality or our level of training, apart from at a very basic level.
AfC Banding (within the NHS) – This could have been a real opportunity to put down some career structure. Instead the bands are often interpreted as relating to managerial skills. Progression through banding is poorly policed and the gateways are ill defined. The fact that they are utilised across all non-medical employees of the NHS means that it is too broad to give real meaning to our career structure. This could have been about clinical skill, but it is not.
HCPC registration/re-registration – Having just been summoned in the last wave of HCPC ‘auditing’ I can say that this is a paper exercise. No one looked at my communication skills or drilled into my reasoning. This is a measure of safety. A poorly policed one at that.
So...
When the Department for Health needs practitioners to fill the gap in GP services, look at the AHP work force and contact the CSP. How on earth do the CSP know if they have the workforce to fulfil these roles? I don’t think they do. I think they have said yes, they’re developing a competency and in conjunction with the universities are putting on training. This seems too reactive with the timescales being too short.
In my last blog I talked about our unique skill set. The ability to appropriately medicalise or demedicalise based upon a patients needs. To offer a public health, rehab, advice and self management message that is positive and enabling. All this could be done at first contact. Let me ask you, of the people working in primary care, how many of your local GP staff have this ability? How much time do you spend undoing the negative implications of previous healthcare interventions?
No body gets MSK like us. MSK is not pain management, its absolutely not orthopaedics. It is about improving MSK health before MSK dysfunction starts, it’s about managing dysfunction within the context of a persons lifestyle. Interventions are often complex and multi-layered, undertaken at one-to-one level or to whole communities. We are good at this. We are the experts.
This is the essence of my argument I think; why has it taken a crisis of funding in the NHS and a lack of GP’s for anyone to think that we might actually be the best at doing this work? Forget about the cheapest. We are the best. We just need to be able to prove this. We need a benchmarked career structure that means something to the decision makers in healthcare. We need to be proud of our profession and we need to be the first choice. We need a leadership structure that acts this way. At the moment it does not. This is my career!!